Yes, in most cases, itching of stitches after surgery is a completely normal and even expected part of the wound-healing process. This sensation is a sign that your body is actively repairing the surgical incision area, producing new tissue cells, and reawakening tiny severed nerve endings. Especially during the postoperative care period after aesthetic surgery, this is considered a positive signal indicating that healing is on track. Correctly interpreting this natural repair signal from the body and distinguishing it from situations that require attention plays a key role in achieving a healthy and successful outcome.
Is Postoperative Itching a Healing Signal from the Body?
Yes, most of the time it is. That itching you feel after surgery is proof of how wonderfully your body’s self-repair mechanism is working. Perceiving the surgical incision as a form of injury, the body declares a kind of mobilization in that area. To understand this process better, think of it like a three-phase construction project.
The Scene and First Response (Approx. Days 1–4)
As soon as the surgery ends, the body’s emergency teams spring into action at the incision site. The first goal is to stop bleeding and protect the area from external threats. Meanwhile, damaged skin cells begin sending out distress signals. Mast cells, which receive these signals, act like alarm bells and release large amounts of histamine into the area. Histamine is the leading actor behind itching. It triggers the itch by stimulating nerve endings in the area. It also dilates blood vessels, helping repair cells reach the site more easily. The slight redness and warmth you see around the wound are due to this. So the early-days itch is actually the result of this intense, well-orchestrated activity at the scene—and it’s completely normal.
The Construction Site and Reconstruction (Approx. Day 3 to Week 3)
Once the scene is under control, the real construction begins. The body works diligently to fill the wound gap. Worker cells called fibroblasts start producing collagen fibers that will form the foundation of the wound. You can think of this collagen as the mortar of the building. At the same time, new blood vessels (new roads) and new skin cells (the building’s façade) are formed.
The most interesting part of this phase is nerve repair. The tiny nerve endings damaged or cut during the incision begin to sprout again in this period, as if laying down new “power lines.” These new nerve endings are incredibly sensitive. As the newly formed tissue contracts and tries to bring the wound together, these delicate nerve endings are stretched and mechanically stimulated. This stretching also causes the itching sensation. In other words, at this stage, the cause of itching is not only chemical (histamine) but also mechanical and neural.
Final Touches and Maturation (From 3 Weeks to 1 Year and Beyond)
The rough construction is finished; now it’s time for fine workmanship. The weak, haphazardly woven collagen fibers formed at the start are gradually removed and replaced with much stronger, more orderly ones over this long process. This allows the scar tissue to take its final form, its color to fade, and its durability to increase. Nerve repair also continues during this period. However, sometimes there can be “crossed wires” when laying these “power lines.” Nerve fibers that carry itch signals may develop more than others or become trapped within dense scar tissue. This is the main reason behind persistent, chronic, neuropathic itching that can continue months, even up to a year after surgery.
What Are the Causes and Types of Postoperative Itching?
To better manage postoperative itching, it helps to recognize its different “characters.” Not every itch originates from the same source. Broadly, we can talk about four types of itch.
The types of itching you may encounter after surgery include:
- Skin-origin (pruritoceptive) itch
- Nerve-origin (neuropathic) itch
- Central system–origin (neurogenic) itch
- Mixed-type itch
Skin-origin itch is the most common and most benign. It arises directly from the healing reaction at the wound site (such as histamine release) or due to skin dryness. In nerve-origin itch, the problem lies not in the skin but in the healing nerves themselves. It is often accompanied by burning or stinging sensations and responds poorly to standard allergy medications. Central system–origin itch, as the name suggests, is a signal coming from the brain or spinal cord. There is nothing wrong in the skin, but the brain sends an itch signal. The most typical example is itch related to painkillers. Mixed-type itch is when one or more of these types occur simultaneously—and this is quite common.
Can the Painkillers I Use Cause Postoperative Itching?
One of the most common questions my patients ask is this. The answer is a clear yes. Especially strong opioid painkillers like morphine are among the most important culprits of severe postoperative itching. This is so common that in medical terminology it’s called “Opioid-Induced Itch.”
How does this happen? Think of it this way: Our brain has a “braking system” that normally keeps itch signals under control and suppresses them. While opioid painkillers relieve pain, they can also temporarily disable this “itch brake system.” When the brakes are off, even itch signals that would normally be too weak to notice reach the brain freely, causing very intense itching, usually generalized and especially concentrated around the face and nose.
That’s why standard allergy medications (antihistamines) usually don’t work well for this type of itch—because the issue isn’t histamine release in your skin. The problem is the release of the brake in your central nervous system. To address this, different medications that directly target this central mechanism need to be used.
When Is Postoperative Itching a Sign of Infection?
This is the most critical question. We now know that some degree of itching is normal. However, there are certain signs indicating that the itch is no longer innocent and may herald an infection. Knowing these “red flags” helps you detect a serious problem early.
Here are key alarm signs that distinguish normal healing itch from an infection requiring immediate contact with your surgeon:
- Itching that progressively worsens and becomes unbearable
- Pain that increases rather than subsides over time
- Redness that extends beyond the incision line and spreads
- Noticeable warmth at the wound area compared with surrounding tissue
- Yellow, green, cloudy, or foul-smelling discharge
- Fever, chills, shivering, or a general sense of malaise
If you experience one or more of these signs simultaneously, the situation is no longer in the “normal healing” category. It indicates your body is fighting an infection and needs urgent medical attention. In such a case, do not delay or try to self-treat—contact your operating surgeon without hesitation. Early intervention is the most effective way to prevent the infection from escalating and causing more serious problems.
Could Rash and Redness Around the Wound Be Contact Dermatitis?
If, in the postoperative period, you notice a suddenly appearing, itchy, red rash—sometimes with tiny blisters—around the wound, one of the first conditions to consider is “contact dermatitis.” This is a reaction your skin develops to a substance it came into contact with during or after surgery and is quite common.
The main suspects that can cause postoperative contact dermatitis include:
- Surgical tapes and adhesives
- Suture materials themselves or their dyes
- Tissue adhesives
- Antiseptic solutions used to cleanse the skin
- Antibiotic ointments applied to the wound
Your skin may show sensitivity to any of these substances. The reaction is usually limited to the area where the substance touched the skin. For example, having a rectangular area of redness and itching exactly where the tape adhered is typical. If you have a known allergy (e.g., to tape or a particular metal), sharing this with your surgeon before surgery is the best way to prevent such a reaction.
Is a Persistent, Months-Long Itch Due to a Scar Problem?
Months have passed since the surgery, your wound has completely closed, yet the itch in that area just won’t let up. If you’re experiencing this, the source is most likely your scar tissue itself. Such long-lasting itching is often part of abnormal scar formation and is neural in origin.
Here are the basic differences to help distinguish hypertrophic from keloid scars:
Features of a Hypertrophic Scar:
- Stays within the boundaries of the original wound
- Raised and red
- Color may fade and it may flatten over time
- Can occur in all skin types
- Features of a Keloid Scar:
- Extends far beyond the original wound margins
- Tends to grow persistently and aggressively
- Often darker, with a purplish hue
- Causes much more intense itching and pain
- More common in darker skin tones and in those with genetic predisposition
Hypertrophic scars result from an exaggerated healing response but remain faithful to the original wound boundaries. They often improve over time and with proper treatments (such as silicone gels and pressure therapy). Keloids are different; they are like benign tumors that grow uncontrollably and spread into healthy skin far beyond the original wound. They are harder to treat and have a high recurrence tendency. In both cases, itch originates from abnormal nerve activity within the scar, and managing this itch is an important part of scar treatment.
What Home Remedies Can Relieve Postoperative Itching?
The good news is that there are many simple and effective methods you can apply at home to manage normal, non-alarming healing itch. These methods form the foundation of itch control.
Here are some practical tips to help you cope with itching:
- Gentle wound cleansing and care
- Keeping the area continuously moisturized
- Applying cold compresses
- Choosing the right clothing
- Drinking plenty of fluids
Gentle Cleansing: Clean the wound area gently as recommended by your doctor. Do not rub—pat dry carefully. Most importantly, no matter how much it itches, never scratch the area with your nails! Scratching both damages the delicate healing tissue and greatly increases the risk of infection by transferring bacteria from your nails to the wound. Instead of scratching, try lightly pressing with a fingertip or scratching the adjacent healthy skin to “trick” your brain.
Moisturizing: Dry skin is itchy skin. Therefore, it is very important to keep the skin around the wound continuously moisturized. Use a hypoallergenic, fragrance-free, alcohol- and dye-free, rich moisturizer. Petroleum-based products like petrolatum (Vaseline) both lock in moisture and create a barrier against friction from clothing, protecting the skin.
Cold Compress: Cold is one of the biggest enemies of itch. Applying an ice pack wrapped in a clean cloth or a cold, damp compress to the itchy area for 15–20 minutes numbs the nerve endings and provides instant relief. You can repeat this throughout the day as needed.
Clothing Choice: Everything that touches the surgical area matters. Avoid synthetic, tight clothing that prevents the skin from breathing and causes friction. Choose soft, loose, cotton garments.
Does Itching Feel Different After Different Aesthetic Surgeries?
Yes, just as each surgery has its own healing process, the character and location of the itching can also differ.
- Breast Aesthetics (Augmentation, Reduction, Lift): After breast surgeries, itching generally arises from two causes. The first is healing of the incision lines under the breast or around the areola. The second—especially after augmentation—is the implant stretching the skin and the sensory nerves beneath it. This stretch stimulates the nerve endings and can cause itching. Friction-related itch is also common in areas where bra straps and bands contact the skin.
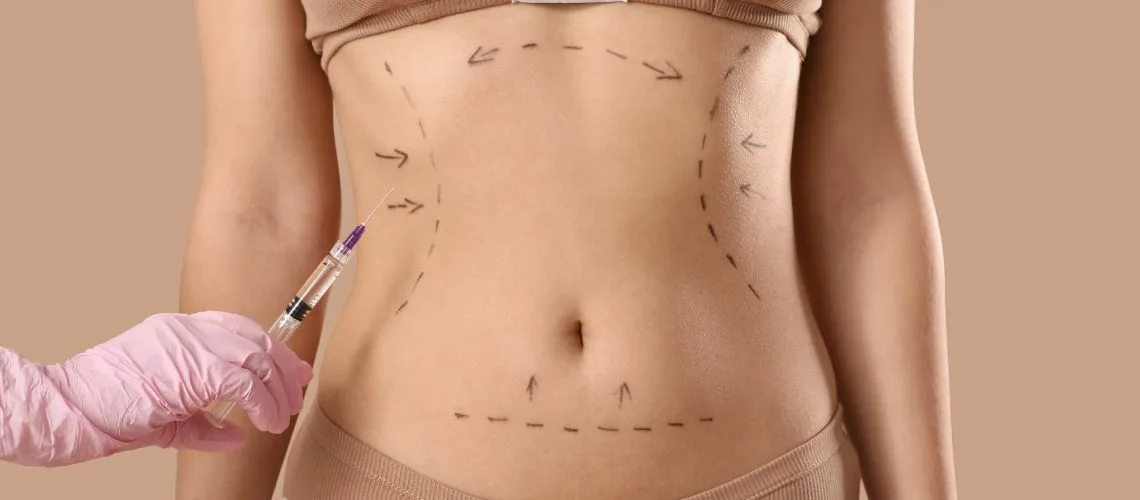
- Body Contouring (Tummy Tuck, Liposuction): Because these surgeries involve very large areas, countless tiny nerve endings try to regenerate simultaneously during healing. Therefore, widespread tingling, pricking, and intense itching—especially starting after the first weeks—are very common after abdominoplasty and liposuction. My patients often describe this sensation as an “itch coming from the inside.” This actually indicates that the nerves are “waking up” again and that healing is on track. Postoperative compression garments can also increase itch by causing friction and sweating. Wearing a cotton, seamless undershirt beneath the garment can ease this.
- Facial Aesthetics (Facelift, Eyelids, Rhinoplasty): The face is one of the areas with the densest nerve network. Therefore, after a facelift, it is very normal to feel itch in front of and behind the ear and along the hairline; after eyelid surgery, along the lash line; and after rhinoplasty, at the nasal tip and dorsum. Stitches in these areas are very fine, tissues are highly delicate, and nerve healing manifests in this way. This itching usually diminishes over time and is a sign that sensation is returning.

Op. Dr. Erman Ak is an internationally experienced specialist known for facial, breast, and body contouring surgeries in the field of aesthetic surgery. With his natural result–oriented surgical philosophy, modern techniques, and artistic vision, he is among the leading names in aesthetic surgery in Türkiye. A graduate of Hacettepe University Faculty of Medicine, Dr. Ak completed his residency at the Istanbul University Çapa Faculty of Medicine, Department of Plastic, Reconstructive and Aesthetic Surgery.
During his training, he received advanced microsurgery education from Prof. Dr. Fu Chan Wei at the Taiwan Chang Gung Memorial Hospital and was awarded the European Aesthetic Plastic Surgery Qualification by the European Board of Plastic Surgery (EBOPRAS). He also conducted advanced studies on facial and breast aesthetics as an ISAPS fellow at the Villa Bella Clinic (Italy) with Prof. Dr. Giovanni and Chiara Botti.
Op. Dr. Erman Ak approaches aesthetic surgery as a personalized art, tailoring each patient’s treatment according to facial proportions, skin structure, and natural aesthetic harmony. His expertise includes deep-plane face and neck lift, lip lift, buccal fat removal (bichectomy), breast augmentation and lifting, abdominoplasty, liposuction, BBL, and mommy makeover. He currently provides safe, natural, and holistic aesthetic treatments using modern techniques in his private clinic in Istanbul.