How Does the Planning and Preparation Process Work Before Breast Aesthetic Surgery?
The success of an aesthetic operation begins long before the scalpel touches the skin, at the planning table. The fundamental rule for achieving an excellent result is proper patient selection and minimization of preoperative risks. Another factor that is just as important to us as technical skill is how mentally and physically prepared the patient is for this change. As surgeons, our primary duty is to analyze whether the result the patient dreams of aligns with medical realities.
Conducting a psychosocial evaluation before deciding on surgery is at least as critical as performing blood tests. The aim here is to manage the patient’s expectations correctly. For example, a patient who hopes to resolve emotional emptiness or social problems solely through a physical change may remain unhappy with the outcome, even after a technically flawless operation. Therefore, we want to make sure that the patient’s motivation is based on a healthy foundation. If expectations are not realistic, postponing or cancelling the operation is the most ethical decision to protect the patient.
In the physical preparation phase, body mass index (BMI) and lifestyle habits come into play. For an ideal healing process, the body must be metabolically balanced. In patients with a BMI over 30, wound healing problems and infection risks are statistically higher. In addition, smoking is our greatest enemy when it comes to tissue perfusion. In a smoker, the capillaries constrict and the amount of oxygen reaching the operated area decreases; this can lead to tissue loss, known as “necrosis”. Therefore, quitting smoking before surgery is not a choice but an obligation.
Risk factors that may lead to postponement or cancellation of surgery include:
- Uncontrolled diabetes
- High blood pressure
- Active smoking
- Morbid obesity
- Blood clotting disorders
- Unrealistic expectations
- Psychological instability
How Is Implant Selection Made in Breast Augmentation Surgery?
The implants used in breast augmentation must be selected in a completely personalized way, according to the patient’s anatomical structure and the result they desire. With advances in technology, we now have implant options with different characteristics. The most commonly preferred material is silicone gel implants, which provide a feeling closest to natural breast tissue. Thanks to their consistency, these implants are very successful at mimicking the natural movement and softness of the breast.
Another option is saline-filled implants. These are placed into the body empty and then filled inside. However, because they may feel like a water-filled balloon to the touch and can develop folds over time, they may not be perceived as natural as silicone gel implants. In addition, the age limits for both types of implants differ; in general, saline implants are recommended for patients 18 years and older, and silicone implants for patients 22 years and older.
One of the questions our patients are most curious about is the lifespan of implants. Although implants are manufactured to be highly durable, they should not be considered devices that are guaranteed for a lifetime. Over time, wear or leakage can occur in the outer shell of the implant. Especially with silicone implants, “silent rupture” can occur, meaning tears that the patient does not notice. To monitor this, in accordance with FDA protocols, regular imaging is recommended starting from the 5th year after surgery.
Implants can be classified according to their surface characteristics as follows:
- Smooth-surface implants
- Micro-textured implants
- Macro-textured implants
- Polyurethane-coated implants
How Are Decisions Made About the Dual-Plane Technique and Incision Site?
The key to aesthetic success in breast augmentation surgery is choosing the correct “pocket” in which the implant will be placed. In the past, implants were placed either completely under the muscle or completely under the breast tissue. However, both methods had their own disadvantages. With subglandular placement (above the muscle), the edges of the implant could become visible, while with complete submuscular placement, “animation deformity” could occur, where the shape of the breast changed with arm movements.
Today, the “Dual-Plane” technique has become the gold standard to eliminate both of these problems. In this technique, the upper part of the implant remains under the muscle, ensuring a soft transition in the décolleté area and hiding the implant edges. The lower part of the implant is positioned under the breast tissue, giving the breast a natural teardrop shape. The Dual-Plane technique is ideal for preserving the natural, slightly downward sloping appearance of the breast and avoiding an artificial “ball-like” look. In addition, by releasing the lower attachments of the muscle, the implant does not remain suspended high up and instead integrates with the breast tissue.
The choice of incision site is critical in order to avoid long-term complications. In particular, we want to minimize the risk of “capsular contracture”, in which the body forms a tight, thick capsule around the implant. Scientific data show that an incision made in the inframammary fold is the safest method. This region provides the surgeon with the best surgical exposure and, because the milk ducts are not disrupted, the risk of bacterial contamination is minimized. With incisions made through the armpit or around the areola, the risk of infection and capsular contracture is statistically higher. Once healed, an inframammary incision lies within the natural crease of the breast and is aesthetically discreet.
The surgical entry sites used are:
- Inframammary fold
- Periareolar (around the nipple-areola complex)
- Axilla (armpit)
Which Techniques Are Used in Breast Lift Procedures?
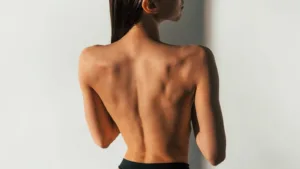
Gravity, breastfeeding, rapid weight gain and loss, and aging all cause the breast tissue to lose elasticity and sag over time. Breast lift, or mastopexy, aims to correct this sagging and restore a youthful and firm breast shape. The technique used, however, cannot be based on a one-size-fits-all approach; it must be determined entirely by the degree of sagging. We evaluate the position of the nipple relative to the inframammary fold using a system known in medicine as the “Regnault Classification”.
In mild ptosis, a “periareolar” incision made only around the nipple may be sufficient. As the degree of sagging increases and the amount of excess skin to be removed grows, more extensive techniques are required. For moderate sagging, a vertical “lollipop” incision is preferred, while for severe sagging, an “inverted T” or anchor-shaped incision is used. The goal is always to achieve the best shape with the least amount of scarring; however, form and long-term stability should never be sacrificed just to shorten the scar.
The most important revolution in modern mastopexy surgery is the abandonment of procedures that rely solely on tightening the skin. Skin is an elastic structure and cannot bear the full weight of the breast on its own; after a while, it will inevitably stretch again. For this reason, we now use techniques known as “dermal sling” or “internal bra”. In this method, a sling system is created from the patient’s own tissue, particularly the deep dermal layers. This sling supports the breast tissue from below and secures it to the chest wall. As a result, the load is borne not by the skin, but by this strong internal structure. In this way, the achieved lift can be maintained for many years. In addition, with a technique called “auto-augmentation”, instead of cutting away the sagging tissue in the lower pole, we reposition it upward to create fullness in the upper part of the breast, allowing for a natural increase in volume without using an implant.
The stages of breast sagging are:
- Mild ptosis
- Moderate ptosis
- Severe ptosis
- Pseudoptosis