Which Type of Anesthesia Is Preferred During the Operation?
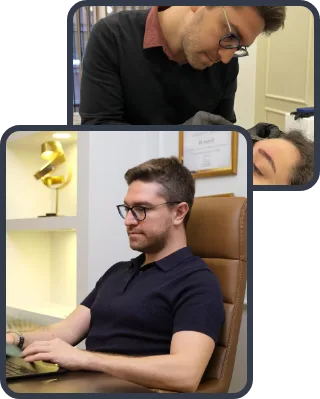
The choice of anesthesia is determined by the patient’s age, psychological state and the surgeon’s preference. In pediatric patients, the unequivocal preferred method is general anesthesia. Otoplasty requires very sensitive, millimetric work, and it is essential that the patient’s head does not move at all during the operation. It is not realistic to expect a small child to lie still for a long time under local anesthesia in the operating room without fear and without moving. In addition, for the child’s psychological well-being, it is best that they do not experience the stress of surgery, do not hear the sounds and do not remember the process.
In adults or in adolescents who are mature enough to understand the procedure, the situation is different. In this group of patients, we generally prefer a combination of local anesthesia and sedation (administration of a sedative via an intravenous line). With this method, the patient is in a deep sleep state, feels no pain, and yet the heavier procedures associated with general anesthesia are not necessary. The recovery period after the procedure is shorter and the patient can usually be discharged much more quickly on the same day. Regardless of the method chosen, the patient’s comfort and safety are always the top priority.
Which Techniques Are Used in Prominent Ear Surgery?
There is no single “correct” method in the correction of prominent ears; the ear structure of each patient is as unique as a fingerprint, and the surgical plan must be individualized. However, the basic principle is always the same: to move the ears backward while preserving a natural appearance and avoiding a “stuck-on” look that clearly shows surgery. In modern surgery, the techniques we most prefer are cartilage-preserving methods based on shaping with sutures rather than cutting and removing the cartilage.
First, the surgical incision is usually hidden within the natural fold behind the ear, so that once healing is complete, there is no visible scar from the outside. If the problem is the lack of the upper fold of the ear (antihelix), we use the so-called Mustardé technique to create an artificial fold by placing special permanent sutures in the cartilage. This procedure is similar to placing stitches in a flat piece of fabric to gather and shape it. If the problem is an excessively deep ear bowl (concha), we use the Furnas technique, in which we pull the ear bowl back by anchoring it with sutures to the firm tissues of the skull base. In most patients, both problems are present to some extent, so we combine these techniques. In some cases, the cartilage can be very stiff and resistant; in such ears, we lightly score the surface of the cartilage to break its resistance and make it easier to shape.
The main surgical maneuvers used are:
- Cartilage thinning
- Placement of permanent sutures
- Cartilage removal
- Excision of excess skin
- Tissue fixation
What Is the Recovery Process Like and What Is the Purpose of the Headband?
After the operation is completed, a special compressive dressing is applied to the ears. This dressing is critically important both for maintaining the newly created shape and for preventing the accumulation of blood (hematoma) under the skin. We usually remove this large dressing one day after surgery and check the condition. From this stage onward, the “headband” or “tennis band” becomes our patients’ most loyal helper.
After the first dressing is removed, we ask our patients to wear an elastic headband. The use of this band is a two-stage process. During the first 1–2 weeks, the band should be worn continuously day and night. It may only be removed briefly during dressing changes or while showering. This continuous use helps to reduce edema (swelling) and keeps the cartilage, which has not yet fully set, stable. In the second stage, it is sufficient to wear the band only at night while sleeping for the following weeks. Night-time use is vital; during sleep, turning over unconsciously may cause the ear to rub against the pillow or fold over, which can strain the sutures and distort the shape. The headband acts as a shield, protecting the ear from such unintended trauma.
The expected conditions during the recovery process are:
- Mild pain
- Swelling (edema) of the ears
- Skin bruising
- Temporary loss of sensation
- Itching sensation
What Are the Risks and Complications of the Operation?
Otoplasty is considered a safe procedure among general surgical operations, with a relatively low complication rate. However, as with every medical intervention, there are some potential risks that patients should be aware of. The most important early complication is the accumulation of blood between the skin and cartilage, called a “hematoma”. This usually manifests within the first 24 hours after surgery as severe, throbbing pain on one side. In such a case, urgent intervention is required to evacuate the blood; otherwise, the blood supply to the cartilage may be compromised.
Apart from this, the risk of infection is quite low when the operation is performed under sterile conditions and with the use of prophylactic antibiotics. One of the late complications that may be encountered is asymmetry or recurrence (partial return of the ear to its former position). Cartilage is a tissue with “memory” and may resist and attempt to return to its original shape. In rare cases, the permanent sutures placed may gradually approach the skin surface over time and become palpable or even protrude; in such situations, a simple procedure to remove the suture may be required.
Possible complications are:
- Hematoma
- Infection
- Wound healing problems
- Cartilage irregularity
- Suture reaction
What Should Be Considered After the Operation?
After a successful surgery, it is very important for the preservation of the result that the patient takes good care of themselves. During the journey home and in the first few days, the position of the head is important. Keeping the head elevated above heart level while lying down (for example, by sleeping on two pillows) helps the swelling to subside more quickly and reduces the throbbing sensation. Lying on the side should be strictly avoided; the supine position (lying on the back) is preferred.
Return to social life is usually rapid; children can return to school after about one week, and adults can generally return to work within a few days. However, there are restrictions regarding physical activities. Because it takes time for the ear cartilage to regain its full strength, contact sports in which the ear might suffer a blow (such as football, basketball or wrestling) should be avoided for at least 1.5–2 months. In addition, for patients who wear glasses, it is recommended to be careful in the first weeks to prevent the arms of the glasses from putting pressure on the suture line behind the ear, or, if possible, to use contact lenses instead.
The points that need attention are:
- Sleeping on the back
- Protection from the sun
- Avoiding trauma or blows to the ear
- Temporarily reducing or stopping the use of glasses
- Keeping the area dry
Are the Results Permanent and What Is the Level of Patient Satisfaction?
Otoplasty is one of the procedures in aesthetic surgery with the most permanent results. The cartilage tissue that is reshaped during surgery takes its final form once the healing process is complete (which varies between approximately 6 months and 1 year) and maintains this shape for life. Although there may be natural enlargement of the ears and loosening of the skin with aging, the ears do not return to their former “prominent” state.
In terms of patient satisfaction, otoplasty is among the most gratifying operations. Especially in children and adolescents, resolving a long-standing self-confidence problem leads to an immediate and clearly noticeable positive change in posture, smile and social relationships. Our patients no longer hesitate to tie their hair back, are not worried on windy days and do not feel the need to hide themselves in photos. This physical change creates a great sense of freedom in the person’s inner world. In short, a properly performed prominent ear surgery at the right time provides not only an aesthetic benefit but also a major psychological contribution to the patient’s life.